Neural EDX ™

The Neural EDX is the first test that measures nerve and motor unit function, and it does this with 100% statistical accuracy/sensitivity.
1918-1944 TESTS WERE DEVELOPED BEFORE IT WAS KNOWN HOW NERVES GENERATE SIGNALS.
A State-Of-The-Art-Review found in insurance company references, Journal of Physical Medicine & Rehab
1. "With standard EMG-type tests it is difficult or impossible to diagnose painful nerve root pathology."
2. "Only if there is obvious muscle atrophy can one be certain there is motor degeneration."
3. "Because studies use severe surgical cases, we are lulled into thinking these tests are specific and sensitive."
Within 15 minutes, all major cervical or lumbar nerves (from specific nerve roots) are tested. The patient is his own control, so accuracy has 100% peer- reviewed statistical sensitivity.
Neospinothalamic A-Delta Fibers – Key To Functional EDX
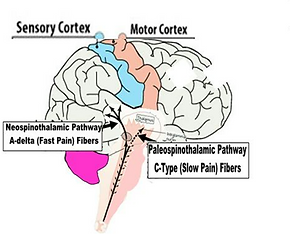

3.5 Million years ago Our reptilian paleospinothalamic system was upgraded by the SRGA2 gene adding the neospinothalamic system with its excellent localizing (Fast Pain) A-delta fibers. Synapsing with spinal cord motor neurons, A-delta fibers trigger the Withdrawal Reflex that moves us away from painful injuries.
2.5 Million years ago our synapses were fine tuned and cerebral cortex expanded by the SRGA2-C gene. In 2000 AD these changes made it possible to measure nerve dysfunction and thereby locate acute and chronic nerve root and peripheral nerve lesions with 94.6% peer-reviewed accuracy.


1963: Hodgkins and Huxley are awarded a Nobel Prize for discovering how nerves and muscles function by way of Voltage-Gated Channels.
1970s: A New Branch of Medicine – Pain Management
How pain was looked upon over the centuries is entailed in the term ‘patient.’ Pain wasn’t something to be treated, but a bothersome symptom the sufferer had to tolerate and be ‘patient.’ In the late 1970s medicine literally rediscovered. Soon Pain Management became a new branch of medicine.
![[GetPaidStock.com]-653cebea9b842.jpg](https://static.wixstatic.com/media/9bd95e_08a4a0ec65484a259907ee78b910dfc8~mv2.jpg/v1/fill/w_380,h_217,al_c,q_80,usm_0.66_1.00_0.01,enc_avif,quality_auto/%5BGetPaidStock_com%5D-653cebea9b842.jpg)


What could go wrong?
The Pharmaceutical Industry
The pharmaceutical industry jumped on board the Pain Train. Absent a reliable method to diagnose the most common pain disorder, radiculopathy, treatment was guided by symptoms. With 50% being referred to health nerve roots, many failures ensued and patients were prescribed pain killers.
Millions became addicts and hundreds of thousands died, and still do, in what seems to be a nation of addicts. It took a few decades for pain specialists to realize that 1944 EMG may be effective at identifying catastrophic large fiber damage, as seen at the end of World War II, but it’s not effective diagnosing slowly progressing degenerative or acute radiculopathy. By the early 2000s EMG was out of Pain and Neurology textbooks.
1944 EMG: An Honest Assessment
Who would refer a patient once they knew 1918-1944 EMG-type examinations:
-
Cannot measure nerve function
-
Cannot in any way assess pain fibers
-
Are limited to large fibers
-
Require two or more adjacent nerve roots to have nearly catastrophic damage or degeneration before detection of radiculopathy is possible?

Why did non-neurologists believe EMG measures function and pain?
Open a text on EMG-type tests and you’re overwhelmed by the complexity of the science. This complexity is unavoidable when measuring a system whose function is unknown. Electrically assessing the structural integrity of nerves is a complex problem.
It’s clear why medical students are not expected to understand this branch of medicine, and why during internships most young interns are admonished to; “Just send patients to the neurologist and read his reports.” The lack of understanding this breeds is such that asking non-neurologists what ‘myo’ in electro-myo-graphy stands for most often the answer is myelin (fatty insulation covering nerve fibers), or myelo (spinal cord). Many are unaware it stands for muscle.
2000: Robert Odell, MD, PhD (Stanford Biomedical Engineering) and James Hedgecock, PhD (Neurophysiology) teamed up and developed the first functional electrodiagnostic device that measures the voltage-gated channels threshold to produce action potentials, f-NCS.



During the acute Epicritic Phase of nerve injury, A-delta fibers up-regulate and synapse with motor neurons triggering the Withdrawal Reflex. Within hours, during the Protopathic Phase, Odell and Hedgecock discovered the A-delta fibers down-regulate. This returns mobility and likely helped our hominid ancestors escape predators, however, this down-regulation can be detected and quantified. The A-delta fibers of an injured nerve requires more voltage to cause threshold action potentials than uninjured nerves. In 15 minutes A-delta thresholds of all the nerves in a region can be measured. The nerve(s) requiring more than average voltage of an electric neuroselective signal determines which nerve(s) is injured.

Neuroselective Frequencies
The world learned how nerves generate signals in 1963, but Over 3 decades passed before Hedgecock determined what was preventing functional measurements. Researchers overlooked two basic factors, a) skin impedance shifts and, b) the skin’s impedance is higher than the minimum voltage threshold causing voltage-gated channels to fire signals. Taking these factors into account, Hedgecock used an AC square wave current as opposed to the DC sinusoidal current researchers had used and patented specific modulations and duty cycles. Then he asked his colleague, Robert Odell, and they collaborated on designing the device, exam algorithms and analysis.
Why Can’t Comprehensive Physical Exams Localize Radiculopathic Lesions?
The medical literature and textbooks only discuss referred organ symptoms, without any mention of referred nerve root pain. However, the consensus of the over 800 physicians who have been certified in A-delta f-NCS, with its 94.6% sensitivity in locating radiculopathic lesions, is that 50% of nerve root symptoms are referred to healthy nerve roots, with half of the 50% feeling pain contralateral side of lesion.


Physical Exams Cannot Localize Nerve Root Lesions
Performing a comprehensive physical examination cannot identify the nerve root causing pain. That’s why the National Institute of Health reports up to 80% of spinal surgeries end with the patient in the same or worse pain and 50% of spinal pain patients developed chronic disability. The Massachusetts General Hospital, Wang Pain Center probably perform pretty good physical exams, but The Massachusetts General Hospital Handbook of Pain Management 2nd Edition states on page 382: “In most cases of low back pain and neck pain, the anatomic and pathologic diagnosis remains unclear.” Most cases, that’s over 50%. The truth is that no text or study has ever found physical examinations are capable of confirming, let alone, localizing radiculopathy.
2002: Randall Cork, MD, PhD, Director Pain Medicine at Louisiana State University, carries out a 2year peer-reviewed study finding the A-delta fiber f-NCS has 94.6% sensitivity locating and quantifying radiculopathic lesions. Cork states; “A-delta f-NCS is the true gold standard, since it’s functional. Pathology is function gone wrong, so abnormal structure can’t be a gold standard. The largest disc herniation I have ever seen was in a cadaver. That’s not pathology.”


Diagnosing Radiculopathy Based on Imaging is Playing Russian Roulette
Nerve function and pain cannot be imaged. Studies have shown that over 50% of symptom free subjects have disc bulging and herniations, so matching imaging to radiculopathic pain is like loading a six shooter with three bullets and playing Russian roulette. Stop and think for a second. In 15 minutes the Neural-EDx™ can locate nerve root lesions with 94.6% sensitivity. If the patient were your mother, father, sister, brother, aunt or uncle what would you use to decide where to treat, inject or operate?
2003: Over 800 neurosurgeons, orthopedists and pain specialists have been certified, since the Randall Cork, Robert Odell and James Hedgecock founded the American Association of Sensory Electrodiagnostic Medicine in 2003.


2005: Medicare Administrative Law Judges recognize the AASEM and f-NCS.

2011 Winning Universal Coverage
Reminiscent of 1970s CT-Scan, which insurers called a ‘billing gimmick,’ Gieco and State Farm paid university professors and presidents of EMG organizations to explain why pain fiber A-delta f-NCS can’t work. This backfired and proved these experts had meager knowledge in basic sensory neurophysiology. A few examples follow.
EMG Expert; “The idea that the skin’s impedance shifts is wrong. The skin’s impedance is fixed and unchanging.”
Rebuttal; “Is it possible the doctor has never heard of the Polygraph? Lie Detectors have been measuring shifting skin impedance since 1924.”
EMG expert; “One cannot stimulate nerve with electricity since there are no receptors in the skin sensitive to electricity.”
Rebuttal; “When this doctor performs a nerve conduction velocity (NCV) he places a stimulus electrode over the nerve, what does he think is passing through the skin to the nerve?”
EMG expert; “If you stimulate the A-delta fibers the patient can only feel pain, because that’s what A-delta fiber transmit.”
Rebuttal; “Next to this statement this ‘expert’ has placed a Guyton & Hall Physiology chart showing the A-delta fibers transmit hot, cold, pressure and hair sensations. In combination with C-type fibers itching sensations are produced. Additionally, recent studies have found electricity receptors in human skin.”
Reimbursement Caveat
For over a decade Medicare has published that both NCS and EMG be performed on the same visit. Medicare Administrative Law Judges have found pain fiber NCS be billed with standard AMA codes. f-NCS/f-EMG payment is reported to ranges between $500 to over $1200. Certification is required, and Medicare recognized certification is included for two doctors with the Neural-EDx™ purchase. Doctor training involves a half day in-office, online power points with an open book exam. Also included is training of up to 2 staff members.

2023: Based on the same principle of activating voltage-gated channels with voltage, Odell and Hedgecock developed F-EMG, which was add to f-NCS in one FDA Class II (Safe & Effective) system, the Neural-EDx™




EMG Experts Misunderstand f-NCS Analysis
EMG Expert; “The A-Delta f-NCS graph is not id different from standard EMG motor EDX, and it does not compare measurements to population averages.”
Rebuttal; “This is comparing Apples to Oranges. Why would one use the same analysis for small pain fiber function as for detecting gross large fiber damage? The doctor is thinking the 1944 EMG must be the superior method. He’s wrong. Comparing measurements to population averages requires categorize patients by age, gender and ethnicity. Each category is analyzed on a Bell-Shaped Curve. The very best possible accuracy is around 65%. In the f-NCS the patient acts as his own control. Because the test is painless and quick all the major nerves are assessed. The f-NCS in the cervical spine has 18 data points, while the lumbar has 14 data points. Since in the vase majority of cases a patient will have a single nerve root involved and rarely 3, by averaging all the measures a Bell-Shaped Curve is representative for that particular patient, which allows detection as close to 100% as statistically possible and independent of age, race and gender.”
Radiculopathy 25% of Doctor Visits
January 2013
Why Patients Visit Their Doctors: Assessing the Most PrevalentConditions in a Defined American Population

Objective:
To describe the prevalence of nonacute conditions among patients seeking health care in a defined US population, emphasizing age, sex, and ethnic differences.


Patients and Methods:
The Rochester Epidemiology Project (REP) medical records linkage system was used to identify all residents of Olmsted County, Minnesota, on April 1, 2009, who had consented to review of their medical records for research (142,377 patients). We then electronically extracted all International Classification of Diseases, Ninth Revision codes noted in the records of these patients by any health care institution between January 1, 2005, and December 31, 2009. We grouped International Classification of Diseases, Ninth Revision codes into clinical classification codes and then into 47 broader disease groups associated with health-related quality of life. Age- and sex-specific prevalence was estimated by dividing the number of individuals within each group by the corresponding age- and sex-specific population. Patients within a group who had multiple codes were counted only once.
Results:
We included a total of 142,377 patients, 75,512 (53%) of whom were female. Skin disorders (42.7%), osteoarthritis and joint disorders (33.6%), back problems (23.9%), disorders of lipid metabolism (22.4%), and upper respiratory tract disease (22.1%, excluding asthma) were the most prevalent disease groups in this population. Ten of the 15 most prevalent disease groups were more common in women in almost all age groups, whereas disorders of lipid metabolism, hypertension, and diabetes were more common in men. Additionally, the prevalence of 7 of the 10 most common groups increased with advancing age. Prevalence also varied across ethnic groups (whites, blacks, and Asians).

Conclusion:
Our findings suggest areas for focused research that may lead to better health care delivery and improved population health.

1944 EMG Diagnosing Acute Radiculopathy
Journal of Neurology: James A Charles, MD, FAAN - 2013
In an article Dr. Charles pointed out the severe limitation of standard EMG in diagnosing acute radiculopathy, upsetting many colleagues. His answer to a particularly angry colleague follows.
“An honest neurologist or physiatrist who is treating patients with spinal traumatic radiculopathic symptoms (STRS) should not have fears that our conclusions will lower their income. However, there are no practice parameters or established guidelines on the clinical utility of EMG/NCS in evaluation of STRS. It appears that unless there is a clinical differential diagnosis including a peripheral neuropathic lesion vs. a root lesion that cannot be resolved with the history, neurological examination, and imaging studies, there is limited evidence to support the use of EMG/NCS in the evaluation, treatment, and prognosis of patients with STRS.”
1944 EMG Diagnosing Chronic Radiculopathy
Physical Medicine & Rehabilitation
State of the Art Review, Vol. 13, No. 2 June 1999, Robert A. Werner, MD, MS and G. D. Cavender, MD EVALUATING RADICULOPATHY: HOW USEFUL IS ELECTRODIAGNOSTIC TESTING?
Page 251/252: “In chronic cases, particularly in individuals with predominantly sensory symptoms, it is difficult or impossible to clinically estimate the type or severity of nerve injury. Only if there is observable muscle atrophy can one know for certain that motor axon degeneration has occurred. The electrodiagnostic (EMG) study can be normal in the face of known pathology.”
Note: It’s even less likely to detect anything in acute lesions.
Page 255: “H wave is named after Hoffman (1918). If used with any regularity it’s in assessment of S1 fibers. Many would argue that the H wave is simply a neurophysiologic ankle stretch reflex and therefore does not have added value in the evaluation of radiculopathy.” F Wave: “Despite the theoretical advantage of using the F response it is of little practical application in the evaluation of radiculopathy, especially a lesion of a single level. If even a few large myelinated motor fibers are preserved, the F wave latency will remain normal. Severe nerve-root damage at multiple levels is necessary to prolong the latency.”
Page 258: “The sensitivities typically reported in the literature are falsely elevated and tend to lull us into thinking that electrodiagnostic evaluation of radiculopathy is both sensitive and specific. Most reports on electrodiagnostic sensitivity used surgical confirmation as the gold standard, although some used imaging. The specificity of imaging studies is low, with up to 50% of asymptomatic subjects having an anatomic abnormality noted on random screening. . . . Using surgery as a gold standard will skew the population tested because they are typically the most severe cases. If only sensory fibers are involved or if the motor involvement is mild the EMG will be normal while the person actually has radiculopathy.”


1944 EMG Medical Texts
The Spine, 5th Ed. Saunders (2006) pg. 218:
“Whenever a patient, whose sole complaint is pain (affecting the limbs, neck or back), is referred for an EDX examination, there is the expectation that there is some concomitant damage to large nerve fibers that will register on the EDX exam. As is noted later, with chronic lesions this is usually an unrealized hope.”
Note: It’s even less likely to detect anything in acute lesions.
Neurology for the Non-Neurologist Lippincott (2007) Pg. 23:
“EMG and NCV in neck shoulder and back pain, in the absence of motor deficit (gross weakness or atrophy), is costly, time consuming and seldom benefits the patient.”
Massachusetts General Hospital Handbook of Pain Management, 2nd Ed. (2002) pg. 353:
“Most neuropathic pain syndromes are mediated by small-diameter pain fibers (C and A-delta), which are not evaluated by EMG/NCV so their value is limited.”
1944 EMG – Pain Management Drives the Final Nail in the Coffin
1944 EMG: Which Nerve Do You Test?
How does one choose a particular nerve upon which to perform an EMG? 50% of radiculopathy pain is referred to healthy nerves, so it shouldn’t be surprising that probably 50% of 1944 EMGs are performed on normal, healthy, nerves. With the 94.6% sensitivity in locating lesions by f-NCS, f-EMG is directed to the involved large fibers and it is not surprising that f-EMG is usually positive, since any injury to any nerve innervating a muscle causes metabolic disturbance that weakens it response to stimulation. While, on top of EMG subjectivity, nearly catastrophic damage is required in multiple adjacent nerve roots before any hint of a problem can begin to be detected. By which time atrophy is so obvious that the diagnosis is clear and EMG is unnecessary.

What Part Does Psychiatry Play in 1944 EMG?
Psychiatry Certificates hang on the wall of all neurologists, because it is a part of neurology. This means they have gone through an in depth study of psychosomatic disorders and placebo effects. In this regard, the following incident gets to the crux of how psychiatric training impacts the thinking of neurologists.
A colleague’s wife had been suffering from lower extremity pain. As did all of the several doctors to whom she was referred, it was suggested that she be referred for an EMG study. One of the last doctors said he only refers patients to “the best neurologist in Newport Beach California.” She agreed and on the appointed day our colleague accompanied her to the Hoag Hospital. During the initial consultation it was pointed out that she has severe atrophy of the left calf that developed after a hysterectomy in which her left ovary had been removed. The neurologist mentioned the atrophy in his report, but he did not explain that this is evidence of advanced left S1 nerve root damage. After the EMG examination, which found nothing, the neurologist explained to his wife; “Your type symptoms are more common with women than men, so it is believed, very likely, these symptoms are associated with hysteria.”
Overlapping muscle innervation is the reason EMG cannot detect single nerve root involvement. Standard 1944 EMG requires two or more adjacent nerve roots have nearly catastrophic damage before detection is possible. Subsequent to this EMG episode f-NCS/f-EMG confirmed radiculopathy of the left S1 nerve root.
Other A-delta Fiber Discoveries
After determining A-delta fiber action potential threshold identifies nerve injury, more data was needed to develop the analysis. To gather this data Hedgecock worked with spine specialists who permitted him to perform the painless, non-invasive f-NCS on their patients.
Following up on a suspicion, Hedgecock asked that the patients all have x-rays in side bending. Generally it is thought that greatest motion between vertebrae occurs during rotation, it doesn’t. The greatest motion between vertebral segments takes place at the limit of side bending. In the cervical spine the first 30 degrees of head rotation takes place between the top two vertebrae, atlas and axis. However, in an adhesion free spine at the limit of cervical side bending the spinous processes symmetrically rotate away from the side of bending. In the lumbar spine the spinous processes rotated toward the side of bending. This is facilitated by proprioceptive elements detecting stretch of the joints on one side and compression on other. These proprioceptive signals are carried by A-delta fibers to centers in the spinal cord that instantly send motor signals directing muscles to position the vertebrae in such as way as to avoid over stretching and over compression. This is a continuous instant by instant process constantly reacting to minute changes.
Hedgecock suspected that since A-delta fibers include some pressure signaling, their down-regulation may disrupt normal vertebral motion. Now he had a chance to see if his theory held water.
In all the patients he found a direct correlation between the f-NCS dysfunction and abnormal vertebral motion. However, in some cases the correlating level did not match the level of symptoms. Hedgecock explained what he had found to the treating doctors and suggested they try treating the non-symptomatic correlating levels to see how this affected the symptomatic levels. In those cases where the doctors followed his advice, the patients reported remarkable improvement in their symptoms at the non-treated levels. Post imaging and post f-NCS demonstrated a return of normal A-delta function and normal vertebral motion.

Experience recommends epidural injections are more effective when the nerve dysfunction is moderate to severe, while facet injection is usually more effective when dysfunction is mild. Experience has logically shown that lesions distal to the nerve root are not associated with abnormal vertebral rotation, while nerve root lesions consistently cause abnormal vertebral motion. The abnormal motion is easily visualized, because it is usually reverse rotation.

Paradoxical Relationship
A few spinal pain specialists have reported that repeat A-delta f-NCS within an hour after injecting Lidocaine does not further reduce A-delta fiber sensitivity. Instead it seems to normalize A-delta sensitivity. This is not conclusive evidence and further investigation is needed.
Contact: PainDx, Inc
Neural EDX ™. This website is not for general public use. It is meant for physician reference only. Nothing presented is meant to represent or imply use other than the FDA Indication and usage. FDA Indications and Usage: The Neural EDX ™ is a diagnostic device that allows the quantitative detection of various sensory neurological impairments caused by various pathological conditions or toxic substance exposures. The subject population for whom this device can be used for diagnostic purposes includes any individual capable of communicating the perception of cutaneous sensation (with the potentiometer, which has a separate FDA clearance, the test is not dependent on the subject reporting perception of the cutaneous sensation, since the action potential of the nerve firing is detectable by the potentiometer). The Neural EDX ™ diagnostic examination may be conducted as part the neurological examination or for screening to detect peripheral neuropathies. Legal Notice DOCUMENTS PainDx, Incorporated. gives permission to use documents on this web site provided that: The PainDx, Inc. copyright appears in copies and a permission notice appear© 2023 PainDx, Inc. Documents from this site are for informational and non-commercial or personal use only. Such will not be copied or posted to any network computer or broadcast or published in any media or method now or hereafter developed, and No modification of any document is made and no unauthorized purpose is prohibited by law. Violation may result in civil and/or criminal penalties. Materials do not use the design or layout of the website. INFORMATION ON PAINDX, INCORPORATED'S WEBSITE INCLUDING SPECIFICATIONS, APPEARANCE AND APPLICABILITY MAY BE SUBJECT TO CHANGE WITHOUT NOTICE. NO REPRESENTATIONS ARE MADE OR IMPLIED AS TO THE SUITABILITY OF THE INFORMATION ON THIS SITE FOR ANY PURPOSE. THE FULL CONTENTS ARE PROVIDED "AS IS" WITHOUT WARRANTY OF ANY KIND AND ARE SUBJECT TO CHANGE WITHOUT NOTICE. ANY TYPE OF RISK WHICH MAY ARISE OUT OF USE OF THIS INFORMATION REMAINS WITH THE RECIPIENT. IN NO EVENT SHALL PAINDX, INCORPORATED BE LIABLE FOR ANY DIRECT, CONSEQUENTIAL, INCIDENTAL, SPECIAL, PUNITIVE OR OTHER DAMAGES (INCLUDING WITHOUT LIMITATION, DAMAGES FOR LOSS OF BUSINESS PROFITS, BUSINESS INTERRUPTION), EVEN IF PAINDX, INCORPORATED HAS BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGES. TRADEMARK NOTICE All trademarks displayed on this website are subject to the U.S. trademark law, which support that any unauthorized use of trademarks is strictly prohibited. Copyright © 2023 PainDx, Inc. - Neural EDX ™ All Rights Reserved.

